
Prof Mason
Liverpool Foot and Ankle Clinic
To book an appointment, either email or phone the number below or click the link.
E-mail: CVDWclerical@outlook.com
Contact Patient Liaison: 07717580737
Flat Foot (Pes Planus)
Pes planus, commonly known as
flat feet, is a condition where the arches of the feet flatten out, causing the entire sole of the foot to come into contact with the ground when standing. It can occur in one or both feet and may be either flexible (where the arch appears when not bearing weight) or rigid (where the arch is always flat).
What are the causes of flat feet?
Pes planus (flat feet) can have a variety of causes, ranging from genetic factors to injuries or medical conditions. Below are the common causes of flat feet:
Congenital Causes (Present from Birth):
- Genetic Predisposition: Some people are born with flat feet, which is often inherited. In these cases, the arches never fully develop during childhood, a condition known as "congenital flatfoot."
- Flexible Flatfoot: This is the most common type of flat feet in children and adults. In this condition, the arch is present when the foot is not bearing weight (e.g., when sitting), but it disappears when standing or walking. Many children have flexible flatfoot, but in most cases, the arch develops as they grow older.
Acquired Causes (Developing Later in Life):
- Posterior Tibial Tendon Dysfunction (PTTD):
- The posterior tibial tendon supports the arch of the foot. Injury or weakening of this tendon can cause the arch to collapse over time, leading to a condition called adult-acquired flatfoot.
- PTTD is the most common cause of flat feet in adults.
- Trauma or Injury:
- Fractures, dislocations, or injuries to the tendons and ligaments in the foot can lead to the development of flat feet.
- Injuries that affect the structure or function of the posterior tibial tendon, in particular, can cause arch collapse.
- Arthritis:
- Conditions like rheumatoid arthritis or osteoarthritis can lead to joint damage and inflammation, which may cause the arch to flatten.
- Flat feet due to arthritis are more common in older adults, particularly in those with inflammatory joint diseases.
- Ligament Laxity:
- Some people have naturally looser ligaments (ligamentous laxity), which can cause the arches to collapse, especially when standing or walking.
- This is common in individuals with conditions like Marfan syndrome or Ehlers-Danlos syndrome.
- Obesity:
- Excess body weight can place additional strain on the arches of the feet, potentially leading to a collapse of the arch over time.
- Age-Related Changes:
- As people age, tendons and ligaments can weaken, leading to the development of flat feet, even in individuals who previously had normal arches.
- The degeneration of the medial foot ligaments and posterior tibial tendon is a common cause in older adults.
- Diabetes:
- People with diabetes are more prone to nerve damage (diabetic neuropathy) and poor circulation, which can affect the structural integrity of the foot, sometimes leading to flat feet.
- Neurological or Muscular Conditions:
- Conditions that affect muscle function or nerve control, such as cerebral palsy, spina bifida, muscular dystrophy, or stroke, can cause or contribute to flat feet due to muscle weakness or lack of coordination.
- Tarsal Coalition:
- This is a congenital condition where two or more bones in the foot fuse together, limiting mobility and potentially causing flat feet. It often becomes noticeable in adolescence when the bones fully form.
- Flatfoot Secondary to Other Medical Conditions:
- In some cases, flat feet can develop secondary to other systemic conditions, such as hypertension or peripheral vascular disease, which can affect circulation and tissue integrity.
Symptoms
Flat feet (pes planus) can present with a variety of symptoms, though many people with flat feet experience no discomfort at all. However, for those who do have symptoms, they can range from mild to severe and often depend on how the condition affects the body’s alignment and mechanics. The symptoms typically worsen after physical activity or prolonged standing. Here are the common symptoms associated with pes planus:
- Foot Pain and Discomfort:
- Arch Pain: Pain along the inside of the foot or arch is common, especially after standing or walking for long periods.
- Heel Pain: The heel may hurt due to increased stress on the plantar fascia, a ligament that runs along the bottom of the foot. This can sometimes lead to plantar fasciitis.
- Ankle Pain: Because flat feet can alter foot mechanics, it can cause strain or discomfort around the ankles, leading to ankle pain.
- General Foot Fatigue: People with flat feet often report that their feet feel tired or achy, especially after long periods of standing or walking.
- Swelling:
- Swelling Along the Inside of the Ankle or Foot: Swelling is particularly common in people with flat feet caused by posterior tibial tendon dysfunction (PTTD). The tendon becomes strained or inflamed, leading to visible swelling on the inside of the ankle.
- Changes in Gait or Walking Patterns:
- People with flat feet may walk differently because their foot mechanics are altered. Over time, this can lead to compensatory changes in walking (gait abnormalities), which can cause pain in other parts of the body, such as the knees or hips.
- Knee, Hip, and Lower Back Pain:
- Flat feet can affect the alignment of the legs, potentially leading to pain in the knees, hips, and lower back. This is because flat feet can cause the ankles to roll inward (overpronation), which places extra stress on the joints up the kinetic chain.
- Difficulty Wearing Shoes:
- People with flat feet may find it difficult to wear certain types of shoes, especially shoes with a narrow or rigid fit. This can cause pain or discomfort, particularly around the arch or ball of the foot.
- Difficulty with Physical Activities:
- People with flat feet may experience difficulty with activities that involve standing, walking, or running for extended periods. The lack of proper arch support can lead to increased fatigue, discomfort, or pain during and after physical activities.

What are the treatments for flat feet?
The treatment for flat feet (pes planus) depends on the severity of symptoms, the underlying cause, and whether the condition is flexible (arches appear when not bearing weight) or rigid (arches are always flat). In many cases, people with flat feet do not experience significant symptoms and may not require treatment. However, for those with discomfort or complications, the following treatment options are available:
Conservative (Non-Surgical) Treatments:
- Orthotic Devices (Arch Supports):
- Custom-Made Orthotics: Custom orthotics are molded to the shape of your foot and can provide support, correct alignment, and help distribute pressure more evenly across the foot. They are often prescribed by a podiatrist.
- Over-the-Counter Insoles: For milder cases, over-the-counter arch supports or insoles can provide additional support and reduce discomfort.
- Supportive Footwear:
- Wearing shoes with good arch support and a firm heel counter can help alleviate pain associated with flat feet.
- Avoid Unsupportive Footwear: High heels, flip-flops, or shoes with poor arch support should be avoided as they can worsen symptoms.
- Physical Therapy:
- Strengthening Exercises: Exercises to strengthen the muscles of the foot, ankle, and lower leg (such as the posterior tibial muscle) can help support the arch and improve foot mechanics.
- Stretching Exercises: Stretching exercises for the Achilles tendon and calf muscles can improve flexibility and alleviate discomfort caused by flat feet.
- Activity Modification:
- Rest: Reducing activities that cause pain, such as long periods of standing, walking, or running, can help alleviate symptoms.
- Low-Impact Activities: Switching to low-impact activities like swimming or cycling can help maintain fitness without putting additional stress on the feet.
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter pain relievers like ibuprofen or naproxen can help reduce pain and inflammation caused by flat feet.
- Icing and Elevation:
- Applying ice packs to the painful area for 15-20 minutes at a time can help reduce swelling and pain, especially after physical activity.
- Weight Management:
- Maintaining a healthy weight can reduce strain on the arches and alleviate symptoms. Excess weight can exacerbate flat feet and contribute to pain in the feet, knees, hips, and lower back.
Advanced and Surgical Treatments:
Corticosteroid Injections:
- For cases where inflammation or tendon damage (such as in posterior tibial tendon dysfunction) is causing significant pain, corticosteroid injections may help reduce inflammation and provide temporary relief.
Surgical Intervention:
- Surgery is typically reserved for severe cases of flat feet where conservative treatments fail, and the condition significantly affects daily life. Surgical options vary depending on the underlying cause:
- Tendon Repair or Reconstruction: Dysfunction of tendons is part of the cause, the damaged tendon may be repaired or reconstructed.
- Ligament Repair or Reconstruction: Dysfunction of ligaments is part of the cause, the damaged ligament may be repaired or reconstructed.
- Osteotomy: This procedure involves cutting and realigning the bones of the foot to create a proper arch, often moving the calcaneum towards the midline, lengthening the outer aspect of the foot or bringing the big toe toward the floor.
- Arthrodesis (Joint Fusion): In cases of rigid flatfoot or when arthritis is present, fusing certain joints in the foot can stabilize the foot and restore alignment.
- Subtalar Arthroereisis: This procedure involves inserting an implant into the subtalar joint to prevent excessive pronation and support the arch.
- Lengthening of the calf: This reduces the excessive pull on the foot, allowing correction.


Flatfoot Surgery
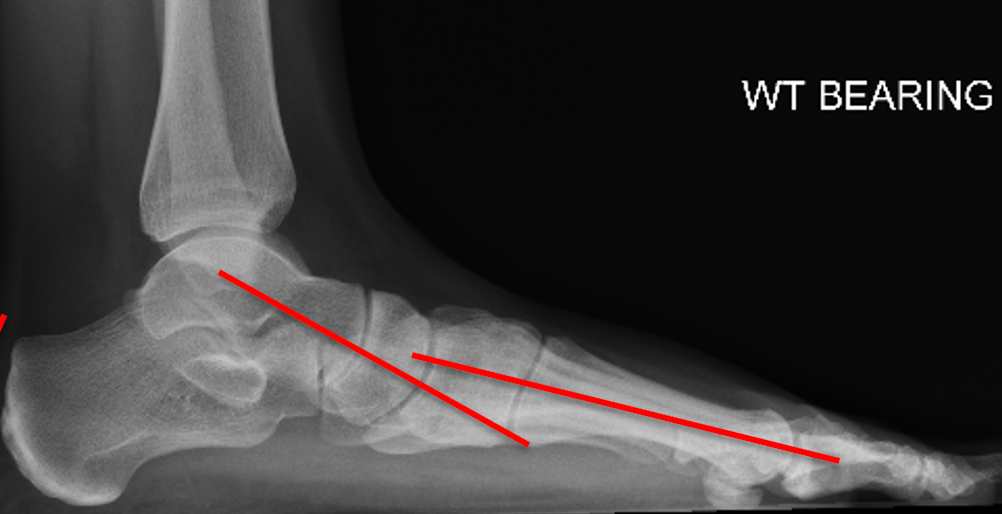
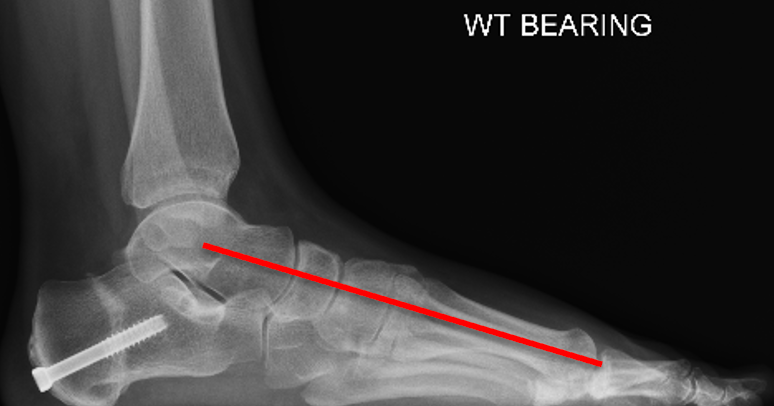
Flat foot reconstruction with gastrocnemius release, spring ligament reconstruction, tibialis posterior reconstruction, calcaneal osteotomy

Flatfoot Surgery
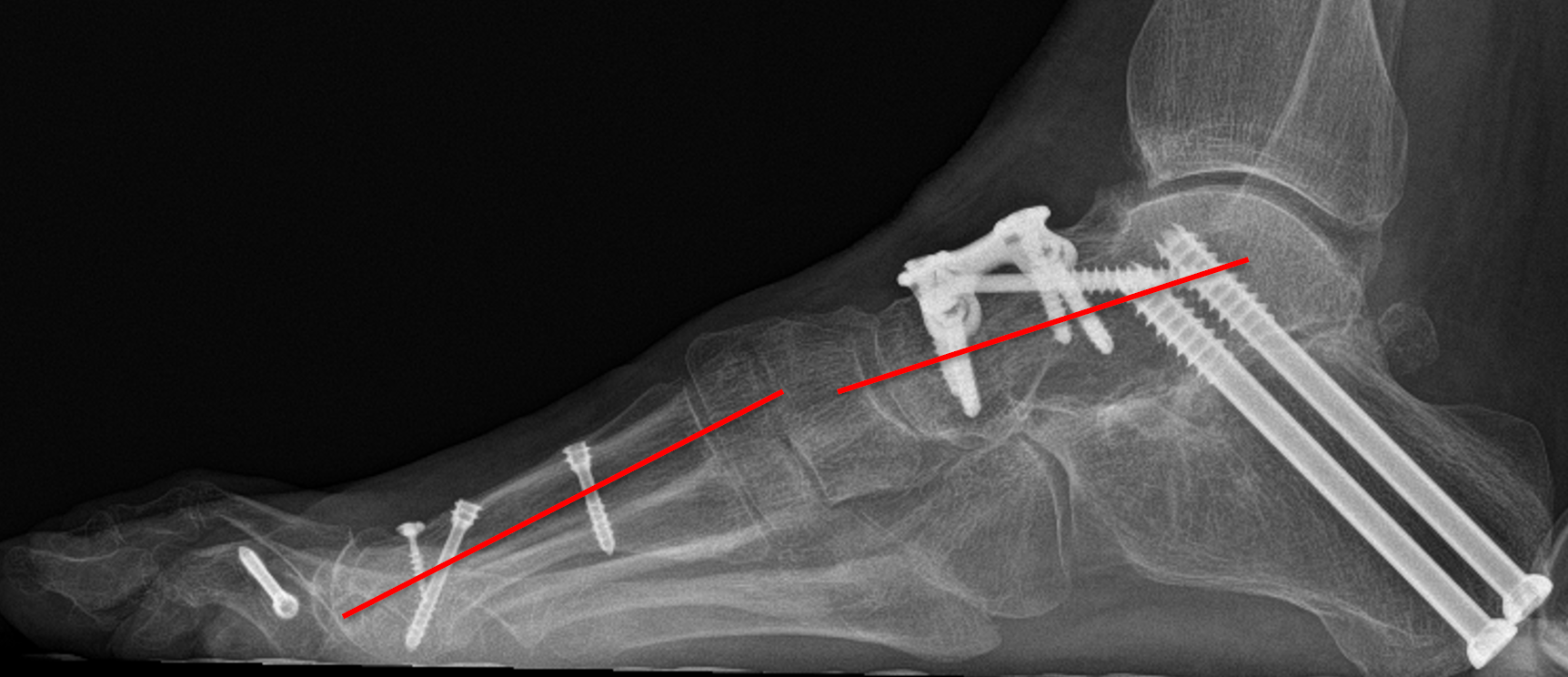
Talonavicular and subtalar joint fusion for flat foot with arthritis.
FAQs
What is the usually recovery following flat foot reconstruction?
Recovery Timeline Summary:
- First 6-8 weeks: Non-weight-bearing with immobilization (cast or boot).
- 2-3 months: Partial weight-bearing and physical therapy.
- 3-6 months: Full weight-bearing, gradual return to normal activities.
- 6-12 months: Full recovery with potential for residual stiffness or mild discomfort in some cases.
What factors may affect recovery?
 Button
Button- Type of Surgery: Simple procedures like tendon repair may have shorter recovery times compared to more complex surgeries, such as osteotomy (bone realignment) or joint fusion, which can require longer immobilization and rehabilitation.
- Age and Health: Younger, healthier patients may heal more quickly, while older patients or those with conditions like diabetes may take longer to recover.
- Adherence to Rehabilitation: Following the prescribed physical therapy and post-operative care instructions is crucial for optimal recovery.

